In 2015, many physical therapists and massage therapists on social media were excited about a study that concluded disc herniation and other physical “abnormalities” of the spine are “part of normal aging and unassociated with low back pain.”
Published in the American Journal of Neuroradiology, the researchers found that “thirty percent of those in their twenties had bulging disc, compared to 84 percent among subjects in their eighties,” based on a review of 33 studies with a total of 3,110 subjects with no pain.
This seems like great news for both therapists and patients. No surgery is needed. No “fixing” required. But we shouldn’t dismiss the biological contributions and evidence for disc herniation and back pain since biology is still pretty relevant in the biopsychosocial model of pain.
There is no strong evidence that massage therapy can guarantee pain relief from a herniated disc or typical low back pain. However, given that pain is a complex experience—not just caused by biological factors themselves—massage may provide some degree of pain relief from the analgesic effects of touch. While current scientific evidence says, “Not really,” some people’s experiences might tell them, “Yes, it works!”
The strongest evidence so far is that massage therapy may alleviate low back pain from disc herniation via descending modulation, a process that involves how your brain interprets sensory stimulation and environmental cues to predict whether you are safe or not. To sort out the mess, we should examine what we know about disc herniation in relation to pain and massage.
What is a herniated disc?
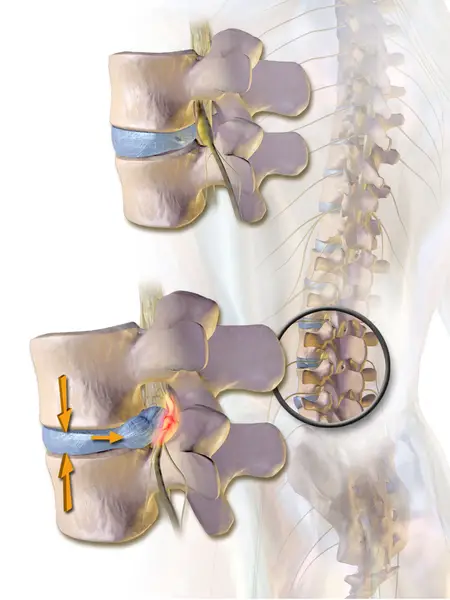
In a herniated disc, the center part of the intervertebral disc—nucleus pulposus—extrudes into the epidural space, which is the gap between the vertebrae and dura matter.
This increases permeability in the blood vessels in the space, allowing inflammatory proteins and markers to concentrate in the area.
The outer ring of the disc, called the annulus fibrosis, has several layers of collagen that look like tree rings and surround the nucleus pulposus.
Since the center contains 70 to 90 percent water (mostly among young adults), this amount gradually decreases with age, a sign of “degeneration.”
Such reductions in disc size has been shown to increase acidity in the discs, which may be caused by reduced metabolic exchange (e.g. exchange of electrolytes between a cell and its fluid environment). This may inhibit cell formation while increasing the number of cell deaths in the nucleus pulposus.
If you had visited your physician or physical therapist, you may have seen a model of the lumbar spine sitting on the counter with jelly-like discs that you can remove and slip them back in like a Jenga game.
But discs cannot slip like that, like a “bar of soap,” as Dr. Jarod Hall said in Physio Network. He said that the endplates hold the discs in place like anchor for the collagen fibers in the disc. “The interesting thing about the vertebral end plate is that there is both a bony and cartilaginous endplate that create an exceptionally strong connection to the annulus of the disc making it IMPOSSIBLE for the disc to SLIP.”
Gene expression and herniated disc
In the past 15 years, research revealed that certain genes may be risk factors for disc degeneration, including disc herniation. Some of these genes are assigned numbers like stormtroopers in the Star Wars universe.
Two of these genes, called COL9A2 and COL9A3, are encoded in a larger protein chain called Collagen IX, which connects collagenous and non-collagenous proteins in various human tissues to keep them stable yet pliable. However, a 2018 systematic review and meta-analysis from Guangxi Medical University in China found such risk factors are not that significant.
Compared to previous reviews, this study pooled data from 10 qualified case-control studies from Finland, India, and several East Asian countries that were more recent and were not included in the recent review. With a total of 2,102 cases and 2,507 controls, they found “no statistically significant association” between the COL9A2 and COL9A3 genes and risk of lumbar disc degeneration.
Even with this finding, the authors pointed out that the studies they gathered had different methods of testing, which may affect the quality of their conclusion.
These include diagnostic criteria for disc degeneration, study design, environmental factors, and language bias (English and Chinese studies were included in this review). This doesn’t mean genetic factors are not potential contributors to back pain with disc herniation, but they may not be as strong influencers as some researchers and clinicians believe.
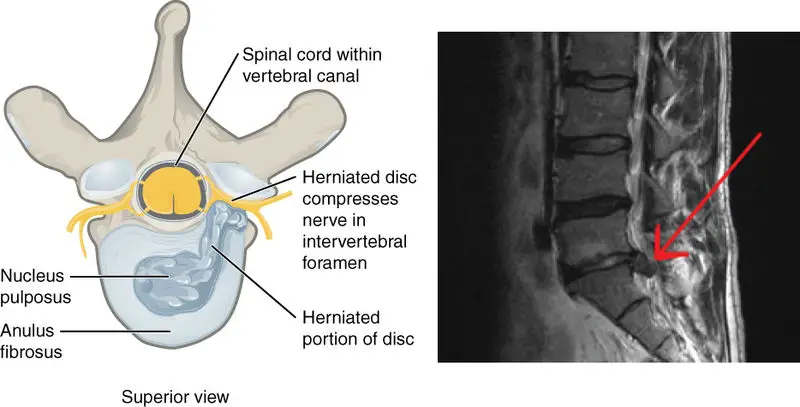
Image: Anatomy & Physiology, Connexions Web site. http://cnx.org/content/col11496/1.6/
Inflammation and bacteria in disc herniation
Inflammation can also be caused by Propionibacterium acnes, a Gram-positive bacteria that has been shown to correlate with patients with disc herniation. But the evidence is pretty weak, according to a recent systematic review that stated, “ …we cannot support that P. acnes and development of symptomatic degenerative disc disease due to the low quality of the results….”
While massage therapy cannot change your genes, “push” a disc back in place, or squeegee bacteria out of your body, it may alleviate the symptoms caused by these factors, similar to most types of low back pain. But be aware that such “degeneration” may not be a significant cause of back pain for some people since research has shown that many older adults with this degeneration are asymptomatic.
Research has yet to reveal why some people have no pain with a disc herniation while some do. Perhaps there is something going on in the brain that affects individual pain tolerance?
Maybe those with a disc herniation and no pain have a healthy lifestyle (e.g. good diet and exercise habits) that suppresses the inflammatory signals? Or could it be that disc herniation just does not elicit symptoms for some people?
For a few lucky folks, a herniated disc could reabsorb back into its place without any interventions!
With the lack the quality research, the best evidence we can fall back on is basic pain science and narrative medicine. These principles can guide therapists and patients on the best approach to less pain and disability and having more independence and locus of control.
These ideas apply to both massage therapy and physical therapy for herniated discs.
Hall mentioned that this change of framework will help patients get back to being physically active and avoid the fear of moving.
“How can we expect patients to succeed if we pump them full of false information that likely creates vivid mental imagery of a spinal disaster?” Hall said. “If we reinforce feelings and mindsets of fragility related to the spine ,we are committing a physical therapy sin. We are breaking our vow to do no harm. We are promoting a scenario that is in contrast to our very name.”
A native of San Diego for nearly 40 years, Nick Ng is an editor of Massage & Fitness Magazine, an online publication for manual therapists and the public who want to explore the science behind touch, pain, and exercise, and how to apply that in their hands-on practice or daily lives.
An alumni from San Diego State University with a B.A. in Graphic Communications, Nick also completed his massage therapy training at International Professional School of Bodywork in San Diego in 2014.
When he is not writing or reading, you would likely find him weightlifting at the gym, salsa dancing, or exploring new areas to walk and eat around Southern California.