Lymph drainage massage (or manual lymphatic drainage, MLD) is a type of gentle massage that is supposed to reduce swelling in the limbs due to fluid buildup. It may help “clear out” congested lymph nodes in a particular area of your body by performing a series of rhythmic, compressive strokes along lymph vessels. Practitioners claim that it can reduce edema, swelling, and/or inflammation from lymphatic disorders or trauma to your body.
Developed as a way to combat lymphedema and lymph system ailments, MLD may be recommended as part of a Complete Decongestive Therapy plan or as part of a post-operative breast cancer or other cancer treatment.
All types of massage involves some sort of therapeutic touch. Unlike a traditional massage like Swedish and deep tissue massage, lymphatic drainage massage focuses on using feather-light pressure and circular movements no greater than the pressure it’d take for your finger to move skin. It also differs from traditional styles of massage because it focuses on the body’s lymphatic system instead of muscles and joints. While traditional methods apply movement as a full-body massage, MLD practitioners work on a specific area or quadrant of the body.
On Instagram, the hashtag for MLD (#lymphaticdrainage) has more than 625,000 posts as of January 2023 and is touted as being one of the top beauty crazes in recent years. Beauty enthusiasts are marketing to those who want to be slimmer and make use of the alleged aesthetic benefits, often with doubtful claims. Is this celebrity bandwagon only good for a passing phase like the current narrative of trigger point therapy, or does it have scientific merit?
Let’s take a look!
What does the lymphatic system do?
Medical research of the lymphatic system has come a long way from early historical observations of the “clear fluid” flowing in the human body. To assess whether or not MLD techniques can be effective, it’s important to have a simple understanding of how the lymph system works.
The lymphatic system has three primary jobs:
- acting as part of the body’s immune system;
- allowing fat and fat-soluble nutrient absorption for digestion;
- maintaining the body’s fluid balance between tissues and blood.
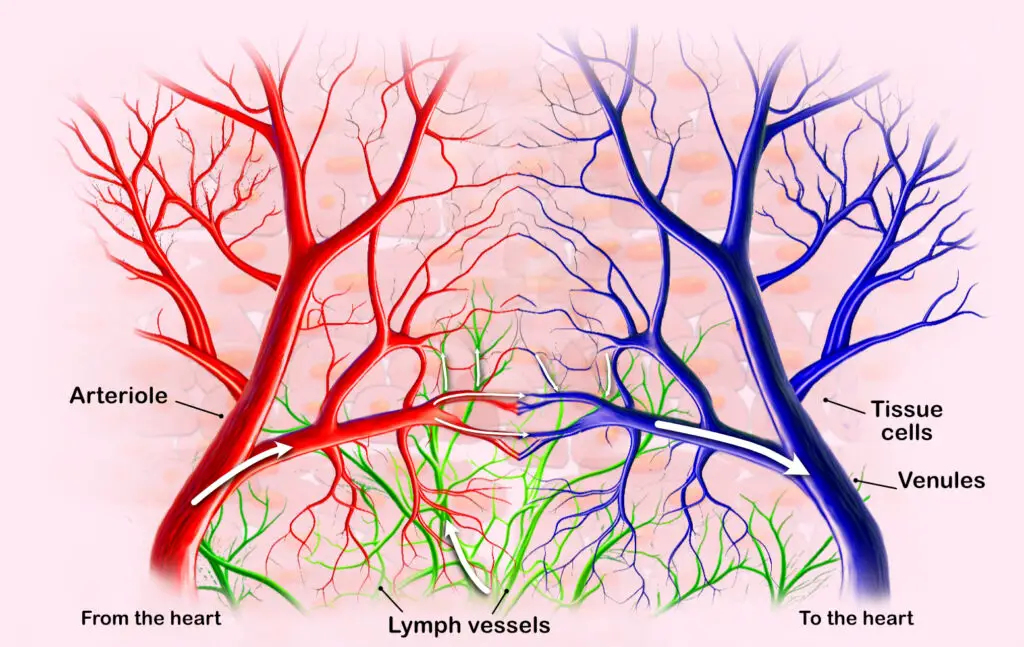
A simplified depiction of how fluids flow from the arteries, through the lymph capillaries, and into the veins, which transports fluids back to the heart. (Illustration by Nick Ng.)
The lymphatic system is comprised of three parts:
- Lymph fluid, which is similar to blood plasma, is made up primarily of white blood cells, an interstitial fluid called chyle (containing fats, minerals and proteins), and other components, including damaged cells and cancer cells. It circulates throughout the body like blood and is a key element in our immune system.
- The lymphatic vessels only carry fluid away from the tissues. Lymph capillaries are the tiny vessels that are found in all body regions, except for the central nervous system, bone marrow, and tissues that lack blood vessels. These small capillaries then form larger vessels, which become even larger lymphatic trunks that drain larger body regions.
- The body has two main lymphatic ducts: the right lymphatic duct, which drains lymph from the upper right body quadrant; the thoracic duct, which drains all of the rest.
Unlike the circulatory system, the lymphatic system doesn’t have a pump, so the lymph fluid moves via pressure gradients from skeletal muscle and respiratory system movements as well as smooth muscle contractions.
Basically, most lymph fluid begins as blood plasma that is forced out of the capillaries and doesn’t get reabsorbed within the capillary beds. The lymph system is built to reabsorb this excess fluid and bring it where it needs to go.
The organs of the lymphatic system include a framework of lymphocyte clusters and connective tissue fibers. These lymphocytes come from red bone marrow and are carried in the blood to specialized organs, which include lymph nodes, adenoids, tonsils, the spleen, and the thymus gland.
When foreign substances get into the body, an immune response is triggered, and lymphocytes multiply and are sent to the affected area to destroy the microorganisms. When a more serious infection occurs, the lymph nodes may swell up and enlarge, which is why this is often checked as a first sign of lymphedema.
Lymph nodes
There are about 600 to 700 bean-shaped lymph nodes in the body that filter and cleanse the lymphatic fluid. They’re usually inside the center of the abdomen and chest, the armpits, neck, and groin. The specialized lymph organs (adenoids, tonsils, spleen and thymus) house specific defense cells for the body that are built to fight infections.
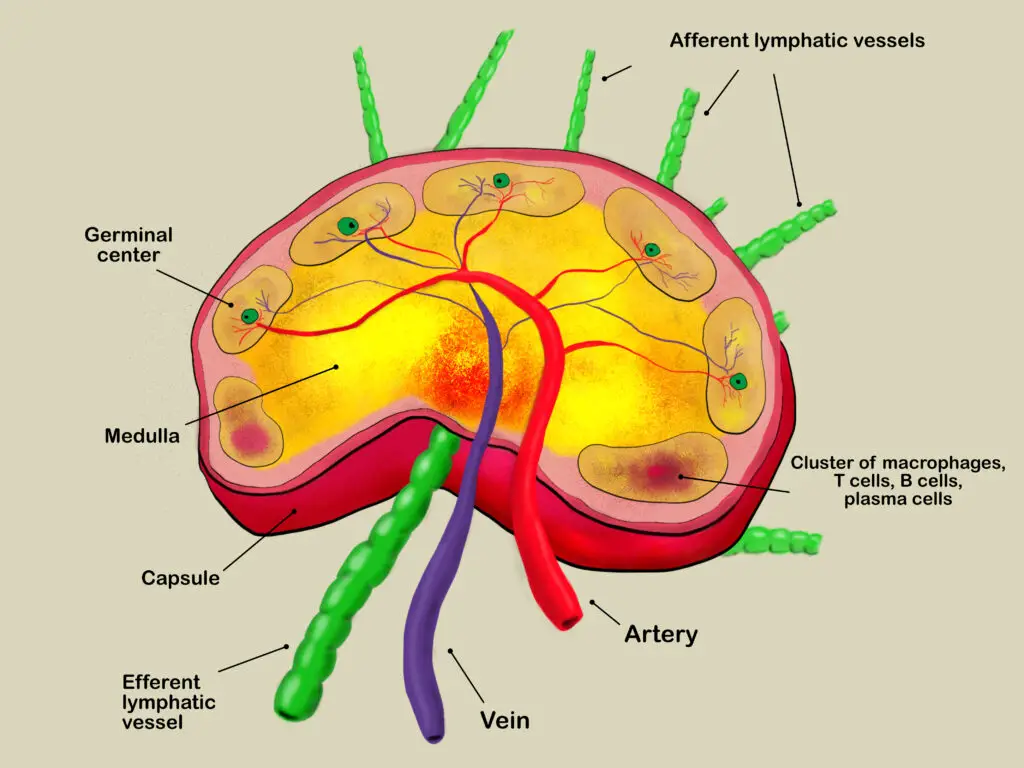
Lymph nodes contain white blood cells that fight infections and filter blood and other fluids in the tissues as they get transported throughout your body. (Illustration by Nick Ng.)
Peyer’s patches line the intestines in a lymphatic tissue network that monitors bacteria in the intestinal walls, and the appendix also has lymphoid tissue to destroy bacteria before it can be absorbed into the intestines.
The lymphatic system not only transfers nutrients but also keeps the fluid balanced within the body. Your body forces about 20 liters of fluid within the capillary system, and only 17 liters is reabsorbed by venous return. The remaining 3 liters becomes the lymphatic fluid, which is eventually returned back to the bloodstream.
If this volume were not returned to the circulatory system, blood pressure would drop, cellular wastes would accumulate, and there would be a decline in oxygen delivery. This backup of fluid would cause edema that could restrict blood flow and result in complications in the body. It’s this potential for fluid backup may appeal to some people of getting a lymphatic massage.
How does lymphatic drainage massage work?
In a healthy lymphatic system, lymph fluid circulates in a one-way trip around the body. It’s transported by lymph capillaries, collected by larger lymphatic vessels, and circulated all the way around to veins near the collarbone (subclavian).
Because it doesn’t have its own independent pump system, the fluid is moved upward against pressure by the pumps created by the active and passive muscle and joint movements. Specialized valves ensure there’s no backflow of fluid.
During this journey, lymph nodes filter the fluid as it passes through them and makes its way to the base of the neck. Once this cleaned lymph fluid reaches the subclavian veins, it’s returned into the bloodstream. And so, MLD assists the flow of lymphatic fluid through the body, which stimulates the lymph nodes and reduces “stagnation” of fluids in specific areas.
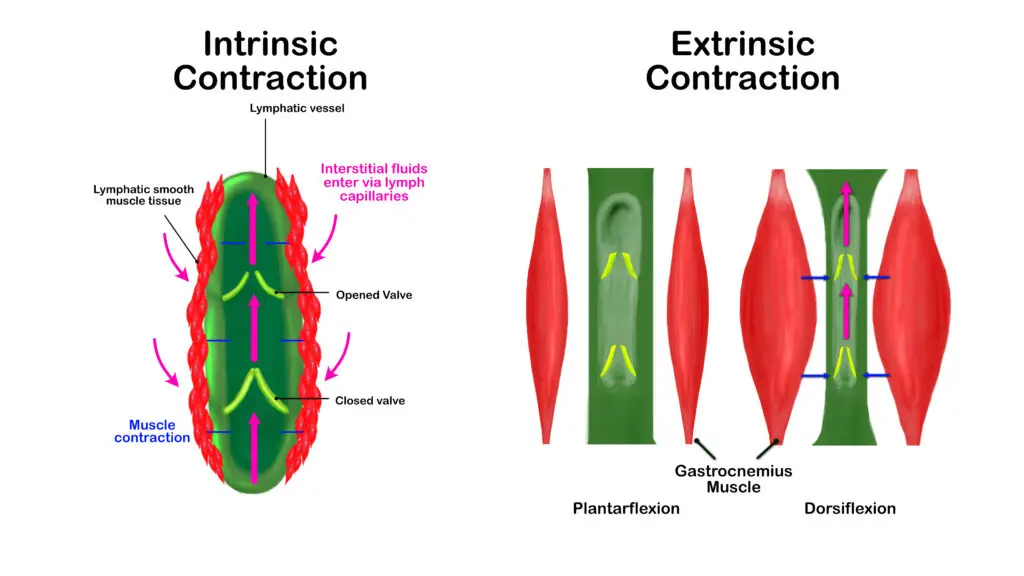
There are two types of contractions that push lymph fluids through our body: intrinsic and extrinsic. Extrinsic contractions tend to occur more on the extremities, especially in the lower body. So one benefit of walking or dancing regularly is to help the lymphatic (and circulatory) system move their stuff around. (Illustration by Nick Ng.)
How to do lymphatic drainage massage
You can do lymphatic drainage massage with four main strokes:
- Stationary circles: These strokes are applied with the palmar surfaces of the fingers or hand, stretching the skin continuously with an oval- or spiral-shaped motion. These movements are typically used on the lymph node areas in the groin or armpits and also on the neck and face.
- Pump technique: Use the entire palm of the hand and upper parts of the fingers to apply circular pressure to the skin. The pump techniques are used mostly to manipulate the lymphatic vessels in the extremities, using one or both hands.
- Scooping technique: Scoops are applied mainly to the body’s lower extremities in a spiral-shaped movement. Palms face up, fingers outstretched (like a scoop), this is a dynamic movement performed with either one hand or alternating hands.
- Rotary technique: This stroke is used on the larger surfaces of the body. The entire surface of the hand and fingers are performed using elliptical movements and applied in a continuous, dynamic way. Typically this is applied with one hand, but like scooping, if both hands are used, it’s in alternating strokes.
According to MLD practitioner Sean Riehl, all MLD techniques have to prevent lymphedema: pressure, direction, rhythm, sequence and contraindications.
- Pressure: Pressure should always be mindful of moving the skin, not the musculature beneath. The touch should be deep enough to deform the skin, but not so deep as to close any of the channels of lymph beneath the skin layers.
- Direction: Lymphatic strokes should always be performed by pushing the lymph toward the correct nodes. Though a therapist would not necessarily do any harm, they would be negating the efficacy of the movements.
- Rhythm: Correct speed and rhythm of the strokes are important to establish a type of pump for the fluid; the initial lymphatics will be allowed to open and shut in a way that the lymph can move down the vessels. Also, rhythm helps to stimulate the parasympathetic nervous system, allowing the client to further relax.
- Sequence: Therapists should always start near the node they are draining the fluid toward, then pushing the lymph toward that node. During the treatment, the therapist will work further away from the node while still pushing the lymph fluid back toward the node.
Caution: As always, the therapist should always keep in mind any contraindications for the session. The goal of MLD is to provide relief to a client, not do further harm.
Typically, lymphatic massages are performed with you lying on your back. Diaphragmatic breathing is used to start and end the session, and the gentle strokes are applied with slow and rhythmic movements. The therapist begins with treating the unaffected lymph nodes and regions first before areas that are congested. Each protocol involves a different number of strokes in a “working” phase of pressure down to a “resting” pressure of zero.
The pressure is often described as one would use to “stroke a newborn baby’s head.” The intention is to stretch the tissue beneath the skin enough to manipulate the lymphatic structures, but not enough pressure to close off the lymphatic valves or affect underlying muscular structures.
Christy Miller, who is a licensed massage therapist and an MLD teacher in Lake Charles, Louisiana, said that it would be impossible to target only the lymph vessels or lymph nodes.
“I think MLD and massage are pretty much the same. They have more in common than not.” she said. “Instead of traversing across the skin like in a typical massage, there’s a push and a little twist [in MLD].”
For years, Miller had been updating her MLD classes the best she could based on both scientific research and client-centered practices. She initially learned this from her mentor Susan Salvo, who is the author of “Massage Therapy: Principles and Practice.” This helps massage therapists to be better informed so that their clients can also be well-informed.
“I think it’s important because when we’re talking about giving the highest standard of care, this includes giving informed consent,” Miller said. “If we’re going to gain consent from a client, then we need to be able to accurately inform them about what it is, what the risks are.”
Is lymphatic drainage massage good for lymphedema?
It’s not clear whether MLD is good for lymphedema or not because there aren’t enough good-quality studies to establish a strong support or refute the benefits.
Lymphedema is an abnormal accumulation of fluids under the skin that becomes so severe that it begins to obstruct lymphatic vessels or lymph nodes. It can be caused by any disease that damages the lymphatic system itself.
Over time, the fluids released from arterial capillaries are incapable of being drained properly, resulting in fluid accumulating under the skin. Most instances of lymphedema occur in the extremities, but it can develop in the breasts, genitals, head, neck, or torso.
Current evidence finds that massage for lymphedema “might not add any effect” to treating or preventing this disease among breast cancer patients, based on a 2020 systematic review of 17 studies. Having analyzed the results by various factors, like the age, sample size, and the type of breast cancer surgery, the researchers found “no benefit to the prevention of lymphedema” compared to other treatments, like compression garments and exercise.
While the technique might not “work” well, the touch itself and having the presence of another person would likely alleviate stress and loneliness that cancer patients often experience.
Lymphatic drainage massage for breast cancer patients
MLD has been featured in several studies in regard to breast cancer-related lymphedema. In one review, the researchers investigated whether or not lymphatic massage would prevent lymphedema in women who had recently had breast-cancer surgery.
Based on 10 randomized-controlled trials with a total of 566 patients, they found “no significant difference in the incidence of lymphedema between the MLD and standard treatment groups.”
The study had limitations in that there were conflicting reports about the efficacy of MLD among the published studies, as well as the “methodological quality of the original studies.” However, the research team concluded that “the current evidence from RCTs does not support the use of MLD in preventing or treating lymphedema.” They added that adding MLD to compression and exercise therapy is “unlikely” to reduce the affected arm significantly.
In 2022, another trial of 194 breast cancer subjects also found “no additional effect of MLD on arm volume reduction and changes in lymph stagnation at the level of the shoulder and trunk” along with other treatments for decongestive lymphatic therapy.
The researchers compared three types of MLD along standard decongestive lymphatic treatment, which includes compression therapy, exercise, education about lymphadema, and skin care. These three groups are:
- treatment with fluoroscopy
- standard MLD care
- placebo group
Across the board, there was not much difference among all groups. “There is no evidence to include (fluoroscopy-guided or traditional) MLD in the treatment of patients with chronic [breast cancer-related lymphedema],” the researchers concluded.
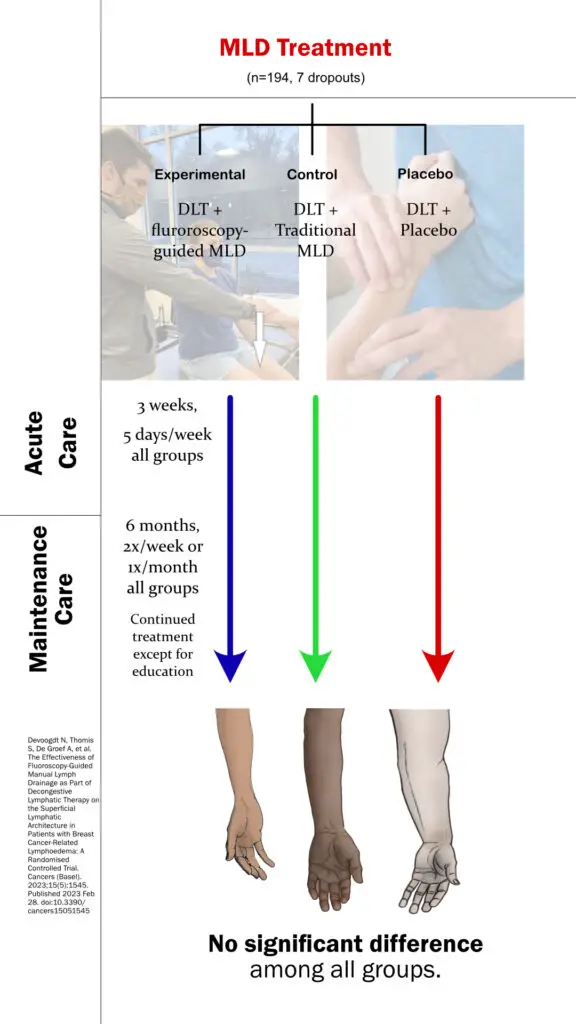
A 2022 study found “no significant difference” in improvement of arm edema between those receiving fluroscopy-guided MLD, traditional MLD, and fake MLD. (Image by Nick Ng)
Can lymphatic massage get rid of cellulite?
Many claims on social media and among practitioners say that lymphatic drainage massage can reduce cellulite visibility, but scientific research finds otherwise. In a 2014 trial, Bianca Schonvvetter et al. studied 15 women (ages 20 to 40) for whether or not there would be significant reduction of cellulite on the skin of their buttocks after consistent treatments of MLD once a week for 14 weeks.
They used ultrasound to measure any changes in affected and treated areas and concluded that “manual lymphatic drainage was safe but not effective as an isolated approach for cellulite management.” The limitations of the study were its small “sample size, low adherence, lack of control and randomization, number and duration of MLD sessions.”
As appealing as it sounds, it seems that the cellulite claim isn’t backed by hard data yet. As of 2023, there isn’t any high-quality research or data that further investigates MLD on cellulite.
Lymphatic drainage massage for sports medicine
Because of the claims that MLD can reduce inflammation and swelling, many athletes would be interested likek they would with sports massage. In 2009, researchers from Pennsylvania State University analyzed 100 peer-reviewed journals and concluded that there is “insufficient and inconsistent ensemble of evidence” to establish clinical guidelines for rehabilitating athletes.
How often should you get a lymphatic massage?
As with any type of massage therapy, there’s no gold standard for how many sessions are recommended. Each client will have individual needs and goals and these should be discussed with the MLD practitioner.
Many practitioners will recommend anywhere from three to five sessions to achieve a particular short-term goal, and then recommend monthly or quarterly maintenance. If clients are working with a medical practitioner for prescribed treatments, this will also be variable. For elective MLD work, each client can discuss with their practitioner what is feasible in regard to schedule, finances, and results.
So does lymphatic drainage massage work at all?
As the previous section’s research show, many studies found little to no additional physiological benefits to standard therapy. While some studies have how positive results, they are limited by poor research methods, lack of control groups, or small clinical samples.
However, these results have not prevented MLD from being prevalently used in medical treatments for edema and lymphedema because it’s such a gentle technique that it’s relatively safe, even if its application is a placebo effect or resulting in positive feelings after treatment.
Miller had a client recently who is a breast cancer survivor and had undergone surgery. But her client felt that she wasn’t well-informed about how to take care of herself afterwards.
“She was scared. She felt that something was happening in her body that she didn’t understand,” Miller said. “I didn’t even do a treatment on her. We just talked, and she just wanted to know more about the lymphatic system. She wanted to be heard, had questions about where her lymph nodes were, and if she could do the massage on herself.
“I think some people just want a compassionate person to keep an eye on it.”
If you seek out this modality for beauty reasons, you need to weigh the realistic aspects of MLD. For example, in MLD and weight loss, look closely at the before-and-after pictures and you may find that there is a reduction in localized fluid rather than actual weight loss. There may be alleviation of bloating and water retention, but these results are only temporary.
Typically, in regard to flushing “toxins” or enhancing lymphatic efficiency, if you’re relatively healthy with an undamaged lymphatic system, you’re already effectively moving lymph, nutrients, and metabolic wastes through your body on their own. It’d be unnecessary to seek out MLD treatment in these situations.
“In all the research that I’ve done, a lot of the assessments that are showing over and over is [massage’s] effect on pain relief, which in the packaging of MLD, the expectation is that it’s gonna be a light massage,” Miller said. “[Clients] want to feel better, they want another set of eyes, they want to be heard—the same that every other client wants from other types of massage.”
Although MLD’s traditional narrative isn’t supported by science, there are merits to increasing patients’ quality of life by offering an overall sense of well-being.
“I think there’s a need for emotional support from an empathetic person,” Miller said. “But just being touched—I don’t feel good, I just had surgery, could you just put your hands on me, tell me that it’s gonna be okay—just show me some love. I think for some people, MLD could be just that.”
What are the risks of lymphatic drainage massage?
As with any massage, it’s important for you to consider any contraindications that you may have before seeking this treatment. If you suspect that you have edema or lymphedema, you should have the approval of your primary medical provider before signing up for massage.
Other contraindications for lymphatic drainage massage are:
- Cardiac problems, including impairments and edema
- Congestive heart failure
- Acute inflammation or infection of any kind
- Blood clots
- Active cancer (it’s important to note that massage cannot spread cancer throughout the body, but contraindications of this sort are often due to risks with chemotherapy and radiation, and sensitivity of the patient)
How to find the best lymphatic massage near you?

A client receives a lymphatic drainge massage treatment from licensed massage therapist Marie Zahn. (Photo courtesy of Marie Zahn.)
The Lymphatic Education and Research Network encourages you to seek practitioners who have completed a minimum of 135-hour training course and are Certified Lymphatic Therapists (CLTs). However, some physicians, nurses, physical therapists, and massage therapists are trained and licensed to practice MLD.
Getting referrals is often useful in narrowing the right therapist for you. These include nonprofit groups, such as the Lymphoedema Support Network and the National Lymphedema Network, who can provide referrals to a qualified practitioner.
Also, ask practitioners how much training they have had, where they trained, and if they have taken any continuing educational courses. The Lymphology Association of North America (LANA) also has a set of standards and guidelines specific to those who are seeking to find a qualified MLD practitioner.
Although there are many appealing benefits to receiving manual lymphatic drainage massage, remember that the clinical efficacy of MLD needs to be studied further. Very few of the clinical trials yield strong data in support of MLD alone in preventing lymphedema in postoperative breast cancer patients. And so, this weakens the case for MLD being an effective stand-alone treatment in reducing swelling and inflammation.
Regarding beauty treatments, its prevention of lymphedema and toning the body are only temporary. Similarly, there’s not enough evidence to prove that MLD is an effective adjunct treatment in sports medicine applications.
If you’re seeking wellness with MLD, chances are, if you don’t suffer from some sort of lymphedema or similar condition, this type of massage would be unnecessary. However, if you enjoy the style for the sake of its gentle quality of touch, there’s generally no harm in receiving it.

Heather Thuesen, LMT
Heather Thuesen, LMT, practices at Wellspring Health in Tioga, North Dakota. She also practiced in Fort Collins, Colorado, since 2014. Her areas of interest and specialization are in athletic and movement work, chronic pain conditions, anxiety-related disorders, and working with adolescents and teens from age 10 to 17.
She is continuing her studies in psychology and PTSD/trauma-related conditions. In addition to creative writing, she has an avid interest in travel, social culture and photography. Her favorite travels involve chasing storms, good coffee, homemade pie and Kerouac-inspired road trips.





