Compared to most healthcare professionals, massage therapists are among the few who spend the most time with patients. They touch them during the entire session, which is typically 30 to 60 minutes long. The nature of the work and environment allows massage therapists and patients to be more engaged with each other during the session.
This potentially develop a better therapeutic relationship. However, more time spent with patients do not necessarily mean better patient-centered care. Sometimes we can default into a “problem-solving” mentality in an attempt to “fix” patients, similar to what the dominant biomedical model in healthcare uses.
In recent years, narrative medicine has been emphasized not only in some medical schools in the U.S., the U.K., and Canada, but also in private practices and international health conferences, such as the International Association for the Study of Pain (IASP).
In fact, IASP presented their first “patient’s voice” in Boston in 2018, which allowed three former patients with chronic pain to share their experiences in living with such pain. Perhaps massage therapy, too, should have a paradigm shift in how practitioners communicate with their patients.
What is narrative medicine?
While it draws heavily from science, narrative medicine emphasizes on the patients’ narrative to help healthcare professionals . It’s developed from several disciplines and schools of thought, including the humanities (philosophy, literary theory, cultural studies, history, ethics, the arts), patient-centered care, biopsychosocial medicine, and psychoanalysis based on the work of psychiatrist Michael Balint.
Dr. Rita Charon from Columbia University in New York City, who is one of the pioneers and advocates of narrative medicine, pointed out that competency in the scientific approach in medicine is not enough because it doesn’t help patients deal with their debilitating condition or find meaning in their suffering.
“…physicians need the ability to listen to the narratives of the patient, grasp and honor their meanings, and be moved to act on the patient’s behalf. This is narrative competence, that is, the competence that human beings use to absorb, interpret, and respond to stories,” Charon wrote in JAMA in 2001.
Narrative medicine “enables the physician to practice medicine with empathy, reflection, professionalism, and trustworthiness. Such medicine can be called narrative medicine,” she wrote.
Rather than having the healthcare profession steer the treatment, narrative medicine allows the patients to participate in the healing process and help the practitioner guide the treatment. In other words, it’s a partnership rather than a top-down chain of command.
The term “narrative-based medicine” (or narrative medicine) first appeared in medical literature in the late 1990s, about 20 years after psychiatrist John Engel proposed the biopsychosocial model of health and disease.
During most of the 20th century, medical practice was highly biomedical, which emphasizes on the biology of the disease with little or no consideration of environment, culture, and behavior that influence a treatment’s outcome.
The framework also teaches medical students to be as objective as possible and to pursue “universal (or near-universal) truths about the causes, treatments, and prevention of disease…,” as Professor Trish Greenhalgh from the University of London said in 2013.
She described narrative medicine as being “diametrically opposite” from the biomedical model. It’s “individual, subjective, perspectival, and relentlessly contextual.” Back then, most physicians in the U.S. practiced with emotional detachment.
However, since the late 1990s, medical practice and education gradually changed as many physicians were learning how to engage with their patients and their experiences. It’s more than prescribing a pill and sending patients out of the office.
Finding meaning with medical narratives
As I was writing this section of the story in a cafe on September 2, 2019, I realized that day was exactly a year since cystic fibrosis activist Claire Wineland passed away a week after a double lung transplant at age 21 due to a stroke.
A native of Los Angeles, California, she was born with cystic fibrosis, a hereditary disease where some cells in her lungs produce too much mucus, which clogs the airways and increases susceptibility to other infections. She was active on social media since 2010, sharing her experiences mostly within the confines of a hospital room.
I knew very little about the disease back then and looked it up online after I read that she passed away in the news. Reading about the of the nature of the disease didn’t ease my sadness I had since it didn’t give me meaning to this young woman’s life.
What gave more meaning to me, and perhaps to millions of people who followed her journey, is her story.
How is the disease affecting her life as she transitioned from adolescence to adulthood? How did she cope when most of her life was confined to a hospital?
How does the disease and environment affect her thinking and self-awareness?
How did her experience and narrative affect others with cystic fibrosis? And what can clinicians learn from her narrative?
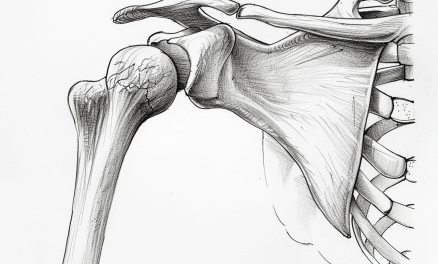
Massage therapists can learn everything there is about pain, from neuroscience to anatomy, but those disciplines by themselves may not give us much meaning to our patients’ experiences.
They can explain ascending and descending modulations that contribute to their back pain, or compare the biomechanics of normal and abnormal gait patterns in walking.
But what do these mean for patients who have low back pain for many years, have sought many treatments that didn’t reduce their pain or disability, and have a hard time working and doing things they enjoy?
Some patients may not be familiar with the narrative medicine approach to massage therapy. Some might engage a little and tell you about their symptoms and point out where they feel it. Some would say little and just want to be “relaxed.”
A few might tell you their deeper reasons on why they came—dealing with a death of a parent, taking care of a child with a chronic illness, or having minor trauma from a recent car accident.
In her book, “Narrative Medicine: Honoring the Stories of Illness,” Charon compared and contrasted scientific knowledge and narrative knowledge. The former “tries to discover things about the natural world that are universally true or at least appear true to any observer,” and the latter as enabling “an individual to understand particular events befalling another individual not as an instance of something that is universally true but as a singular and meaningful situation.”
Also, narrative medicine looks at “individual human beings grappling with the conditions of life” and “attempts to illuminate the universals of the human condition by revealing the particular,” while non-narrative knowledge “attempts to illuminate the universal by transcending the particular.” Neither is better than another. Both are needed in practice.
The four divides of narrative medicine
Currently, there is no universal definition of narrative-based medicine, but many researchers and clinicians are trying. Charon described it as medicine practiced with the capacity to recognize, absorb, metabolize, interpret, and be moved by stories of illness.”
In 2014, a group of international experts in Rome, Italy, agreed that narrative-based medicine is “a fundamental tool to acquire, comprehend and integrate the different points of view of all the participants having a role in the illness experience.”
While these are pretty broad terms, narrative medicine is more about the individual—the unique experience and narrative that each person carries. Thus, it is challenging to pinpoint a specific definition of narrative-based medicine when there are so many variables that constitute the practice.
However, some experts have identified characteristics that makes up narrative medicine. First, Charon identified “Four Divides” that cause a disconnection between the patient and the clinician:
1. Relation to mortality: Clinicians and patients have a different viewpoint on death, especially if the patient is terminally ill or is fighting to keep breathing for many years.
Oftentimes, the clinician is the healthy one to the patient’s perspective (how else could they take care of the sick if clinicians themselves are sick?) and may be more aloof to the patient’s perspective on mortality.
While many massage therapists do not to work with patients who are in near-death conditions regularly, “mortality” can be replaced with diseases, stress, and injuries.
2. Context of illness: Clinicians see illness and pain as a biological phenomenon, while patients see them as something that changes their life: how they function, what is their role in society and family, etc.
A disease or injury can change patients’ behavior and how well or poor a treatment can be.
For example, cultural and religious factors can influence how compliant patients are in taking a medication for certain mental diseases. Some scientists hypothesize that being involved in a religious activity and being among a tribe can lower depressive symptoms, which makes such patients more likely to stick with the medication plan well.
In massage therapy, patients may perceive back pain as something that changes how they work, interact with their children or spouse, or participate in their favorite sport or activities. Depending on the patient they work with, therapists should adapt their explanation of pain differently to each individual.
3. Beliefs about disease causality: Charon mentioned that clinicians see an explanation of a disease through “replicable scientific evidence,” while patients may view it based on their personal experience, family lore, or magical thinking or beliefs.
She gave an example where a clinician see epilepsy as “abnormal foci of electrical activities in the tissues of the brain,” while Hmong parents of their young daughter might see it as “ancestral spirits ‘unable to settle down’.”
Massage therapists may have already encountered this often in practice when patients tell them that their low back pain is caused by an “unstable sacroiliac joint” because their chiropractor or physiotherapist told them so.
4. Shame, blame, and fear: As part of human primal behaviors, both clinicians and patients sometimes show these emotions during a consultation and treatment.
Clinicians may be fearful in asking some personal questions pertaining to their patients’ health and lifestyle, while patients may be embarrassed to share certain parts of their lives and behavior. This emotional tug-o-war can affect the outcome of a treatment.
For example, some patients might feel vulnerable and uncomfortable to share their health history to a therapist of an opposite gender, and the therapist might miss out an important element that can affect the quality of the treatment. Contrarily, some therapists might blame a poor treatment outcome on patients for whatever reasons rather than exploring why such an outcome happened.
The 7 C’s of narrative medicine
While the Four Divides addresses the problems in a typical clinical encounter, the Seven C’s zero in on the details on how we should communicate with our patients. Developed by Dr. John Launer, who is a general practitioner and family therapist and teaches at Health Education England in London, the Seven C’s help bring out the patients’ narrative and help clinicians understand the underlying problem and take precautions in how they communicate.
Conversation: This is seen as a treatment itself rather than a mean to a treatment. The goal is not to solve the problem but to moving forward to a “problem dissolution through the creation of new stories” by helping the patient think about their problem in different ways. This usually happens during the consultation, and having a conversation puts the patient and the therapist “on a level field.”
Curiosity: This does not equate to “prying” or “being nosy.” Instead, being curious about a patient’s problem involves finding out why they came to see the therapist.
Circularity: This concept moves the therapist away from a “linear” approach of thinking about the patient’s condition (x causes y). Instead, circularity refers to recognizing that some patterns in human health is an “endless, three-dimensional dance without perceptible beginning or end,” similar to the Kreb cycle or feedback loop in the nervous system for persistent low back pain.
The patient’s story is endless cycle of interactions throughout his/her life that contribute to their symptoms. Circularity offers potential change in the patient’s narrative about their condition, building an alternate narrative with different possibilities.
Context: Ten patients may come to you for their low back pain problem, but without the content of their condition, their symptoms may be indistinguishable from each other since therapists tend to think low back pain as mostly a biological or structural problem. A patient’s narrative on their condition likely stem from multiple narratives: the media, previous therapists, prior beliefs, family, and friends.
This also applies to therapists who have narratives of our own, stemming from our education, practice, biases, and scope of practice. Being aware of how context drive the patient-therapist interaction is crucial during a treatment. Otherwise, we might end up treat those ten patients the same way like an assembly line.
Co-Creation: Tying the previous C’s together, co-creation involves both the patient and the therapist to weave their stories together to create new ones. This is not a “share and tell” session.
Like in Conversation, co-creation helps the therapist be a participant and a guide of the Conversation. This process gets the therapist to be a participant instead of being detached from the patient’s condition.
Caution: Sometimes the narrative medicine approach can backfire, creating more distress for the patient, especially if the patient is seeking the therapist for help within the therapist’s practice (e.g. massage, exercise), not talk therapy. Therapists should be mindful when asking about personal matters.
Care: A basic trait of all that narrative medicine needs, we need to keep this in mind—as Dr. John Launer wrote, “Without which nothing else works.”
“Lifespan psychologists and developmental psychologists have stressed the importance of considering illness as a non-normative transition of life, which requests the individual to work towards the re-establishment of the normative life balance.
“When a person faces a chronic illness, the need to reconstruct their life story connecting the past life with the present experience of illness is strong.
“In this particular context, narrative becomes an opportunity to give voice to the disruption and to provide it within a time framework not separated from the other life events which form part of the individual’s autobiographical story.” ~ Fioretti et al.
What’s holding back narative medicine in massage therapy?
“I think one of the biggest obstacles in both clinical education and practice has to do with both time and value. Most practitioners believe that implementing narrative medicine principles will take an inordinate amount of time during a clinical encounter,” Pam Ressler said in an online interview with Massage & Fitness Magazine. She is a registered nurse and a faculty member at Tufts University School of Medicine in Boston, Massachuetts.
“ I think one reason is that initially integrating narrative-based medicine may be perceived as time-consuming, and in the U.S., payment is usually procedure-based, and not time-based. This will continue to evolve, but I think this is a barrier. Another reason is that narrative medicine invites some vulnerability for both the clinician and patient, as we deeply observe the human experience.”
Physical therapist James Stark from Bronson Healthcare System in South Haven, Michigan, said that even the biopsychosocial framework of health is lacking in his profession. No one seems to know how to use it in practice.
“I suspect that this is because the concepts are so nebulous and there is not a consistent algorithm to follow,” he said. “The role and value of listening and connecting seems to be left out as the time constraints are significant and algorithms are easier to understand. Narrative medicine is a method that helps clinicians get to the heart of the experience of pain and, as such, it acknowledges a [biopsychosocial] perspective.”
Ressler explained that clinicians who have been trained in narrative medicine have better patient outcomes when they align the care plan with patients’ values and goals. Even so, there is still another obstacle: the skepticism of narrative medicine in clinical care.
Thus, narrative medicine is not taught in many nursing, physical therapy, and medical schools.
Although she admitted there’s a lag in modernizing healthcare education, Ressler is optimistic that narrative medicine will be a requirement in the 2020s and beyond.
“As clinicians and those involved in healthcare see a greater number of individuals with chronic versus acute conditions, the necessity of integration of narrative-based practices will become more essential in their overall treatment of illness and restoration of health and function,” Ressler said.
Stark gave an example of how he used narrative medicine in practice.
“Recently, I said to a new patient, ‘I am ready to hear your story now. I want to hear about you, your life, your back pain, and how those things interact,’” Stark said. “Her reply was insightful, and this was the most efficient four minutes of exploration of her issue that I can imagine. When I repeated that story to one of my colleagues, he told me that he would never dare ask that question because the electronic medical record that we use requires so much data that just listening would not allow him to get the required information into the system in an efficient manner. That is a huge barrier.”
“Another barrier is social,” Stark added. “It is uncomfortable to hear someone’s story when you do not have an answer to the stated or implied question ‘What do I do to fix this?’ We are not trained to be comfortable with uncertainty. We are trained to have answers.”
Is narrative medicine outside of scope of practice?
Some clinicians may argue that asking patients to share their stories and explore their beliefs are stepping over their scope of practice. While practicing narrative medicine does have a fine line that clinicians tread on, they can still do so without violating their scope of practice.
Ressler argued that the concepts of narrative medicine fits well within healthcare professionals’ scope.
“Rita Charon describes narrative-based medicine as medicine practiced with narrative competence ‘to recognize, absorb, interpret, and be moved by the stories of illness.’ This definition can be applied to disciplines other medicine within healt hcare without overstepping scope of practice,” Ressler said. “One’s experience with illness is different than simply the diagnosis of a disease. By learning to listen and observe in a specific way, our insights into understanding the context of a patient’s illness can be amplified and strengthened.”
Dr. John Lauer said that healthcare practitioners are not curious enough when working with patients. Patients’ narratives help them avoid making wrong assumptions about the patients.
“The essence of a narrative approach is to try and enter the other person’s way of looking at the world and go with it,” Launer said. “If someone wants a practitioner just to ‘do things’, then just do them! But people from all cultures have stories to tell, and if they meet a professional who is genuinely interested in these stories, they will nearly always share them.
“My advice is: show an interest, back off if anyone doesn’t seem to like it, but try it again when they trust you more.”
What if narrative medicine backfires?
Because of their previous experience with health care professionals, some patients may not want to open up with massage therapists and just want to be “work on.” As Launer said, perhaps that is the best approach to go at the moment. If they return to see you repeatedly, then it may be an opportunity to investigate their issue a little more.
In such scenarios, Stark suggested a strategy.
“David Butler and Lorimer Moseley talked about people whose beliefs are set in sandstone, in sandcastles, or single grains of sand,” Stark said. “Those whose concepts are set in sandstone are very challenging to work with, but remember, even sandstone wears away bit by bit. If you can create a therapeutic alliance, by really listening and empathizing with them, by accepting their story, acknowledging that their concept makes perfect sense from their perspective, sometimes you can get them to accept that there is a different perspective that is also possible. I hope this new perspective is one that can give an actionable plan which includes increased patient autonomy.”
Stark finds that the “the sandstone fixed ideas ” are less common among patients who have been living in pain for a long time.
“[They] would love it if you were able to ‘fix’ them, but they are wary and distrustful as they have heard this so many times before, I confess that I cannot ‘fix’ them,” he said. “I generally follow up by asking, ‘Why would you expect me to fix you when no one else has been able to?’ Then I ask if they are interested in my help in exploring options to help themselves. Their narrative often allows me much greater access to areas where they are willing to go in this direction.”
A word of caution: narrative medicine is not a one-size-fits-all approach nor is it a stand-alone intervention. Ressler said that practitioners must be sensitive to culture nuances and how much each patient prefers to share their narratives.
“Use of narrative medicine should always be culturally based, and be layered upon the clinical care being delivered. Many chronic conditions cannot be ‘fixed’ but can be treated and managed effectively,” Ressler said. “While this is not the answer most patients and families want to hear, it is part of the narrative and important for the clinician to pick up on. Narrative medicine is not only helpful for understanding the patient but also for understanding our own frustrations, values, and goals as a clinician. Deep observation in a narrative framework helps a clinician understand and examine how their goals may align or not align with a patient’s.”
Piggybacking on Ressler, Launer mentioned that narrative medicine can help clinicians work with patients who are raised from a different culture than their own. From the teachings of the Canadian psychiatrist and anthropologist Laurence Kirmayer, Launer learned about the “contest of interpretations” that clinicians should avoid.
“If [patients] insist on their interpretation and I insist on mine, we will get nowhere,” Lauer said. “If I can show an interest in their stories as individuals – how they got to where they are, what happened on the way, what elements contributed to their condition and so forth – their own story may begin to change and so will my story about them. Every narrative has its own internal energy if you don’t try to take it over. That doesn’t exclude doing things as well. You can give an injection or other physical treatment and still continue the conversation.”

Photo: Nick Ng
Allowing patients the time and space to tell their story during a consultation is already a therapeutic process, and such interaction often is a sign of trust development. However, massage therapists are not counselors, psychologists, marriage and family therapists, or any related professionals and should not attempt to cosplay one.
Even if one is, the patient is seeking massage therapy for help, not talk therapy. What therapists can do is to ask questions, listen, and give appropriate touch during the session. They should not give our opinion about their situation nor should we interject their story with ours. (“Oh, that happened to me, too!”)
“Connecting with the human in front of us is never out of our scope of practice: it is the heart of our practice.” ~ James Stark, PT
A native of San Diego for nearly 40 years, Nick Ng is an editor of Massage & Fitness Magazine, an online publication for manual therapists and the public who want to explore the science behind touch, pain, and exercise, and how to apply that in their hands-on practice or daily lives.
An alumni from San Diego State University with a B.A. in Graphic Communications, Nick also completed his massage therapy training at International Professional School of Bodywork in San Diego in 2014.
When he is not writing or reading, you would likely find him weightlifting at the gym, salsa dancing, or exploring new areas to walk and eat around Southern California.





Great article, I’ve been thinking about Narrative Medicine a lot this last month and it’s great to have a thorough overview. How we can best use elements of NM in Massage Therapy is an important consideration.
Hi Jessica. Great question. There is no one-size-fits-all approach for each client or patient. Narrative medicine is an evolving process, like revising an essay or telling a story on film. Oftentimes, it is simply listening to them and acknowledging their narratives. Just don’t cosplay a psychologist or family therapist.